Chronic kidney disease (CKD) is a slow-moving disease that prevents the kidneys from functioning properly. The main function of the kidneys is to filter the blood in order to remove waste and excess water from the body in the form of urine. When their capacity decreases, these wastes accumulate, which can cause many complications.
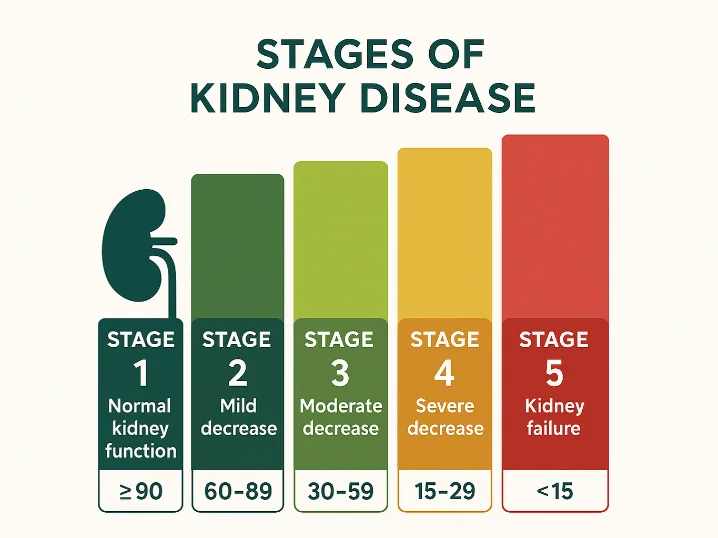
This disease is divided into 5 stages, depending on the severity of the renal involvement. These stages are determined by an indicator called DFG, which assesses how well or poorly the kidneys are functioning.
The DFG: a key indicator
GFR, or glomerular filtration rate, is an estimate of how much blood the kidneys filter every minute.
The higher this number, the better the kidneys work. Conversely, the lower it is, the more renal function is impaired.
How is GFR measured?
The GFR is not measured directly, but calculated from:
creatinine levels in the blood (a waste produced by muscles),
age,
sex,
and sometimes weight.
A normal GFR is greater than 90 ml/min/1.73 m².
Based on this benchmark, people can be classified into one of the five stages of CKD.
The five stages of chronic kidney disease
Each stage corresponds to a level of kidney function. The more advanced you are in the stages, the more damaged the kidneys are.
Stage 1: Normal kidney function with warning signs (DFG ≥ 90)
At this stage, the kidneys are still functioning normally but there are signs that they may be affected:
Presence of protein in urine (called proteinuria),
Anomalies visible on ultrasound,
Or family history.
Symptoms: often none.
What to do.
Monitor the evolution,
Monitor blood pressure,
Control blood sugar (blood sugar levels),
Adopt a good lifestyle.
Stage 2: Slight decrease in renal function (GFR between 60 and 89)
The GFR begins to decline, but symptoms are still rare or absent. Mild kidney damage is often found in routine blood or urine tests.
What to do:
Avoid medications that are harmful to the kidneys (e.g., some anti-inflammatory drugs),
Continue to manage diabetes or hypertension well,
Avoid tobacco and alcohol.
Stage 3: Moderate (GFR between 30 and 59)
This stage is often divided into:
Stage 3a: GFR between 45 and 59,
Stage 3b: GFR between 30 and 44,
At this level, the function of the kidneys is really impaired, and symptoms may begin to appear:
Possible symptoms
Persistent fatigue
Swelling of the legs or ankles (called edema),
Muscle cramps,
Anemia (lack of red blood cells),
Itching,
foamy urine.
What to do:
Be followed up by a nephrologist (kidney doctor),
Have regular blood and urine check-ups,
Adjust diet (less salt, sometimes less protein),
Prevent cardiovascular complications.
Stage 4: Severe illness (DFG between 15 and 29)
At this stage, the kidneys are functioning at less than 30% of their capacity.
Frequent symptoms
Nauses,
loss of appetite,
Difficulty sleeping,
Intense itching,
Shortness of breath,
Blood pressure difficult to control.
What to do:
Plan with the medical team: dialysis or transplant if the situation deteriorates,
Be very rigorous with treatments and diet,
Avoid infections and overexertion.
Stage 5: End-stage kidney disease (DFG < 15)
At this stage, the kidneys are almost not filtering at all. This is called end-stage renal failure.
Waste material accumulates in the blood, which can become life threatening.
Severe symptoms
Problems of concentration,
Confusion,
Severe nausea,
Vomiting,
Intense shortness of breath,
Decreased urine production,
Uncontrollable hypertension.
Possible treatments:
Dialysis: a treatment to filter the blood artificially (3 times/ week in hospital or at home),
Kidney transplant: if compatible and healthy for undergoing it,
Comfort care (palliative) if others
options are not possible or desired.
CKD is slow-moving, but can be detected early with a simple blood test.
It’s essential to know your GFR and monitor it regularly, especially if you are at risk (diabetes, hypertension, family history).
The earlier your kidneys are treated, the more you can slow down the progression and avoid dialysis
Adopting a healthy lifestyle, following your treatments properly, having regular checkups, and seeing a specialist if in doubt can really change the course of your illness.
HEMOFAB’s commitment to kidney health
At Hemofab, we understand how crucial kidney health is, especially for people on dialysis or requiring specific medical follow-up. Our mission is to develop innovative solutions to improve the quality of life of patients with renal failure.
Protect your fistula with the FAV Protector
If you are on dialysis, it is essential to protect your AVF from infection and trauma. The FAV Protector, designed by Hemofab, is an innovative solution to ensure your safety and improve your comfort every day.
👉 Discover our solution and order now: FAV Protector
To go further
We will continue to publish a series of articles on kidney failure, its treatments and best practices for preserving your kidneys.
💙 Take care of your kidneys, they take care of you!
📩 Sign up for our newsletter to receive our tips and stay informed about kidney health.